The Great Unwind: Changes coming to Medicaid eligibility
Three years since the beginning of Covid, the pandemic’s classification as a public health emergency and its subsequent continuous eligibility for Medicaid recipients is coming to an end. The end of the emergency will pose a challenge to Texas on two fronts:
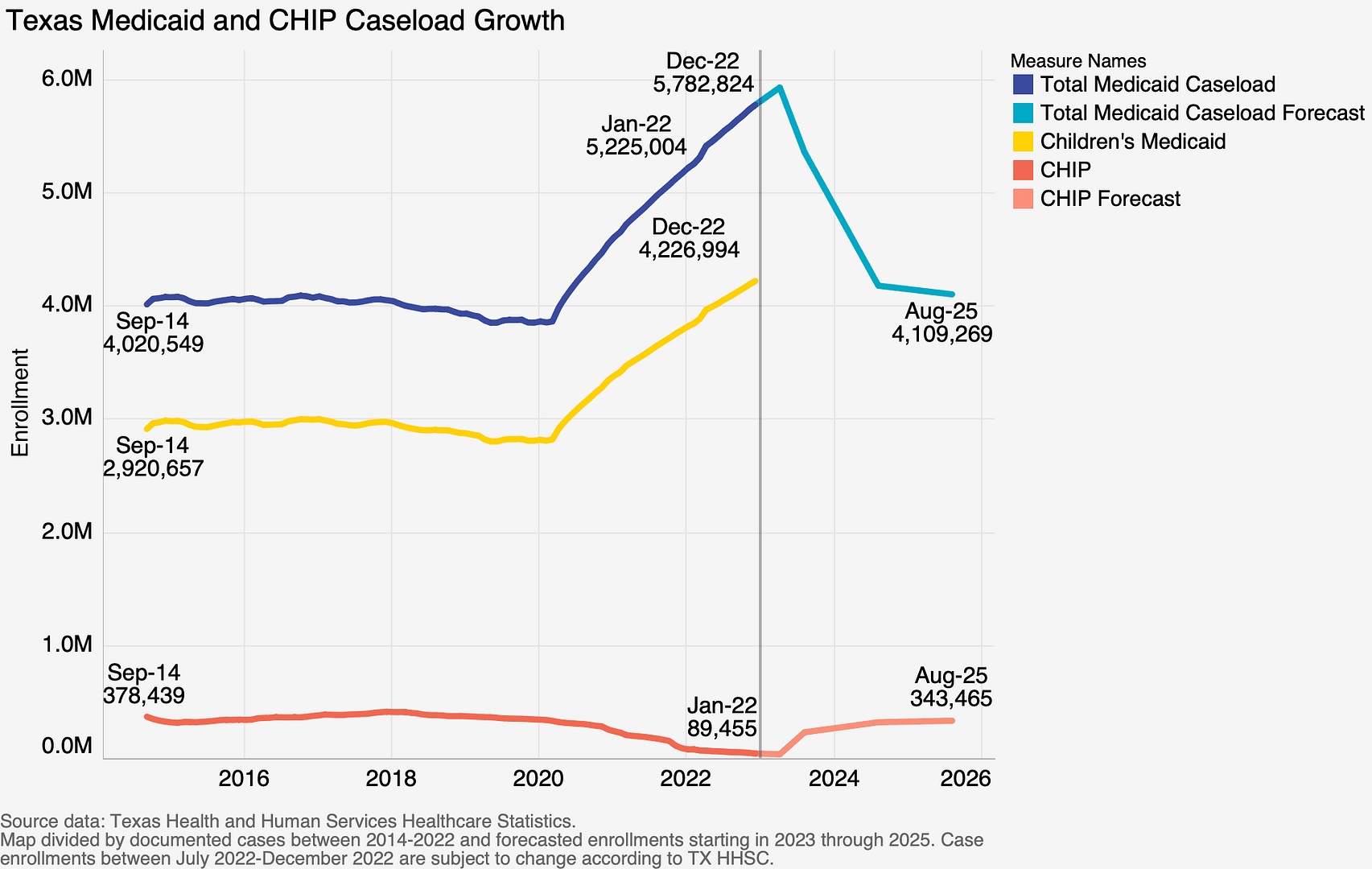
- All of the nearly 6 million Medicaid and Children’s Health Insurance Program enrollees will need to have their eligibility for the programs fully reassessed.
- The state’s uninsured rate is going to jump when Texans are inevitably dropped from the Medicaid rolls.
 Medicaid and CHIP eligibility
Medicaid and CHIP eligibility
The Health and Human Services Commission is responsible for reassessing the Medicaid and CHIP eligibility of nearly 6 million Texans. This tremendous undertaking will be, in part, dependent on an aging IT infrastructure and a workforce of front line workers that has suffered in recruitment and retention during recent years.
To maximize the efficiency of the process, the Health and Human Services Commission will prioritize redetermining eligibility for the 2.7 million Medicaid and CHIP recipients who were either flagged as potentially ineligible or have not updated their information with HHSC during the course of the pandemic.
The agency will process cases in three cohorts, beginning with those who are most likely to have lost eligibility during the pandemic:
- Women who were pregnant,
- Young people who have aged out of Medicaid; and,
- Adults who no longer have a dependent in their home.
This process has already begun, and the first disenrollments will become effective on April 1, 2023.
While hundreds of thousands of Texans have likely legitimately lost their Medicaid eligibility, inevitably, some eligible Texans will be disenrolled due to administrative “churning”, which occurs when enrollees fail to return paperwork on time, or have out of date contact information on their account. In fact, the U.S. Department of Health and Human Services estimates that 15 million people nationwide will lose Medicaid and CHIP coverage, and nearly 7 million of those disenrollments will be due to churn.
The good news is that with this foresight, the federal and state governments can take action to prevent these erroneous disenrollments. The Health and Human Services Commission is prohibited from disenrolling a client without attempting to contact them using multiple modalities — text, email, voice, mail — and the agency has made a $143 million request to the Texas Legislature to hire 642 temporary staff, improve the state’s 2-1-1 resource system, and strengthen the IT system that manages eligibility.
More uninsured Texans?
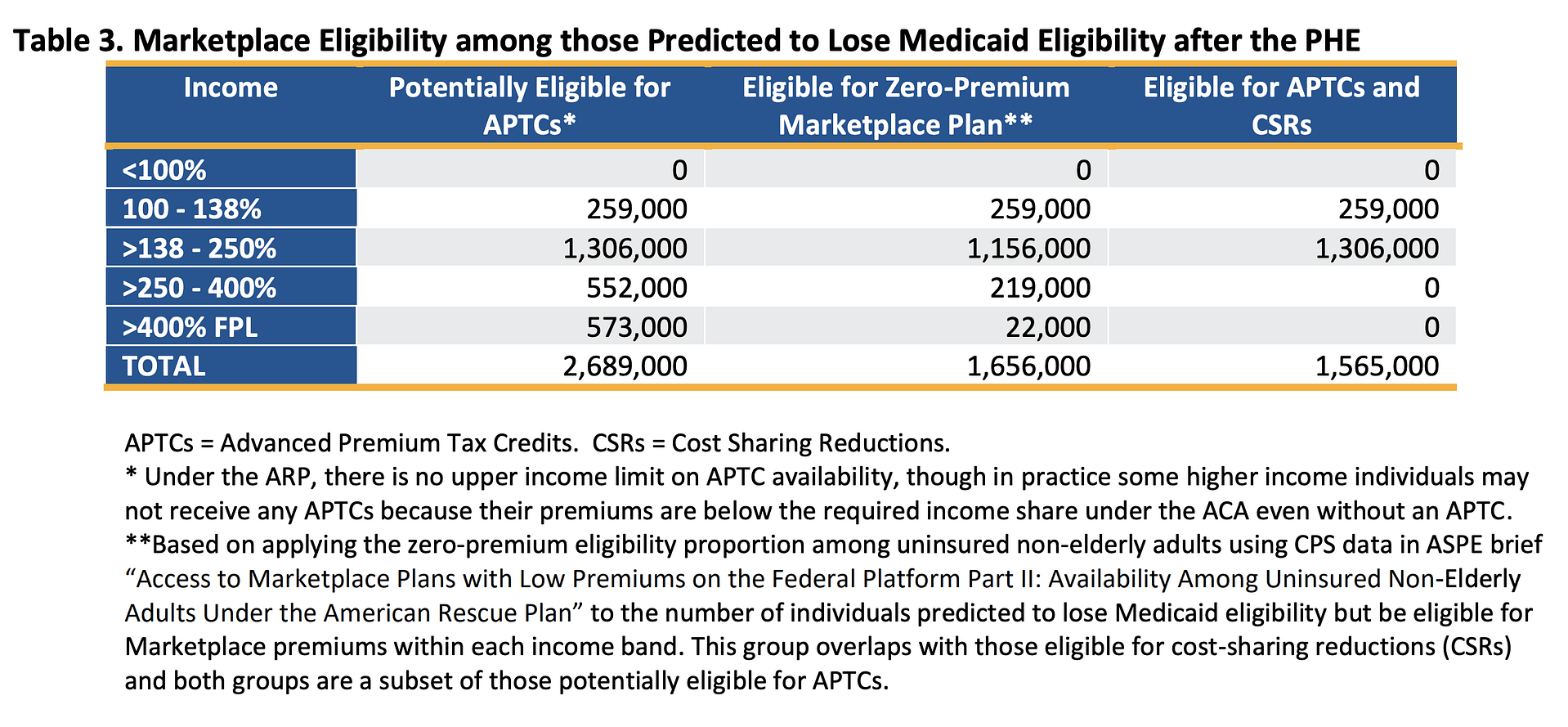
At the end of this months-long redetermination process, the state of Texas will face another obstacle — a group of uninsured Texans, some, who after aging out of Medicaid, have never had to shop for health insurance. The state of Texas should seize this moment and direct this population to the Affordable Care Act Marketplace where the overwhelming majority will be able to find subsidized health insurance, with most of those eligible for zero cost premium plans. The U.S. Department of Health and Human Services has produced a chart outlining predicted ability of disenrolled Medicaid clients to find affordable coverage on the Marketplace.
How can we ensure that the process of moving from Medicaid to private insurance goes smoothly?
Texas 2036 Senior Policy Advisor Charles Miller testified in front of the Senate Finance Committee on ways to do just that.